Making strides towards a world without tuberculosis
Dr Lucica Ditiu, Executive Director of the Stop TB Partnership, tells Health Europa Quarterly about the ongoing global effort to combat tuberculosis.
The Stop TB Partnership was founded in 2001 to pave the way to eliminating tuberculosis (TB) as a global healthcare concern by ensuring that swift, high-quality diagnosis and treatment are made available for everyone who needs it. It is currently working towards the objectives outlined in its Global Plan to Stop TB 2018-2022, a costed five-year roadmap for a co-ordinated worldwide response to the continuing TB epidemic. Dr Lucica Ditiu, Executive Director of the Stop TB Partnership, tells Health Europa Quarterly about the ongoing global effort to combat tuberculosis.
What are the key goals outlined in the Global Plan to Stop TB 2018-2022?
We have developed a number of plans for a longer-term vision for combating tuberculosis. The World Health Organization (WHO) has developed an overarching strategy to end the TB epidemic by 2030. The Stop TB Partnership devises more specific, targeted strategies in three- or five-year increments, with the current plan covering 2018 to 2022 – this period aligns with the goals of the United Nations’ (UN) 2018 High-Level Meeting on Tuberculosis, which established very concrete actions and deliverables.
The primary objectives of the Global Plan to Stop TB include:
- Cumulatively diagnosing and treating 40 million people with TB by the end of 2022;
- Implementing preventive treatment for 30 million people; and
- Cumulatively diagnosing and treating at least 1.5 million cases of drug-resistant TB.
The Global Plan also incorporates targets for transforming the responses of governments and healthcare providers to tuberculosis, to centre those responses more closely on the rights of people; by ensuring gender-sensitive care, by ensuring that there is no stigma associated with TB, and by ensuring that any person with TB will have access to diagnosis, treatment and care. There are also commitments in place with respect to research: the aim is to secure funding of $2.1bn per year for research into tuberculosis diagnosis, vaccination and treatment. We also need to secure funding for the entire programme, which costs around $30m per year.
The final commitment is related to accountability: essentially, making continued progress on combating TB is the responsibility of everyone, starting with heads of state and government, and then continuing down to every single person affected by TB – this is a collective effort.
Is the world on track to meet those goals by the end of 2022?
The very clear answer to that question is no – if anything, we are now further away from reaching the target. 2018 and 2019 were relatively good years in terms of work around TB; there were some good achievements made and we had a realistic hope that we might be able to reach our targets. Unfortunately, 2020 really turned our efforts upside down, largely because of COVID-19; and now not only are we not on target to reach our goals for 2022, but in terms of the TB crisis and the work that is needed to address it, we are effectively back in the year 2010.
We saw a sizeable drop in the number of people, including children, with TB and drug-resistant TB who were diagnosed and treated in 2020 as compared to 2019; and unfortunately, that still appears to be the case in 2021. There need to be significant efforts made to push countries back to where they were before the pandemic, but unfortunately that is not happening in a lot of places. We are not on track in terms of coverage or in terms of financing: funding for non-COVID-19 areas of healthcare has suffered in a lot of countries, because funds have been diverted from areas such as TB to treat and combat COVID-19. We are also not on track to reach our commitment for TB research – not only has COVID-19 disrupted funding for research projects, but because the majority of clinical trials relying on patient participation were on hold for most of 2020, and even now they are greatly reduced.
We have observed that a lot of advances which had been made on human rights and stigma reduction with respect to TB have been effectively rolled back as a result of the COVID-19 pandemic. Because TB and COVID have similar symptoms, we have seen a lot of people feeling stigmatised, embarrassed, scared and lonely. It is a very difficult situation.
What significant factors affect the prevalence and distribution of tuberculosis? Is systemic inequality an issue?
The numbers of people with TB are relatively high in Asian countries with large populations, such as China, India, Indonesia or the Philippines. If we look at numbers of cases per 100,000 people, we still have high percentages in the Asian countries, but we also see high proportions in a lot of the African countries. Around the 1970s and 1980s, everyone believed that TB had been or would soon be entirely eliminated; and so people effectively forgot about it for a decade or so. Within that period, the virus quietly grew in several parts of the world, including in some populations in the richer countries; then New York had a huge problem with TB in the early 1990s.
TB is everywhere; that is the issue. We cannot be safe from it – it is similar to COVID-19 in that sense. The number of people with TB is significantly smaller in high-income countries, but there are still a lot of cases in low- and middle-income countries; and even in the higher-income countries it can be particularly prevalent where there are pockets of poverty. London has a very high number of people with TB, for example: a few years ago it had similar rates of TB to some of the African countries; and it was known as the capital of TB in Europe.
The situation has changed a bit now, because the vaccine for COVID-19 is now being distributed in almost all countries around the world; but until very recently, if you placed a map of high TB incidences over a map of the places in which we did not have full penetration of COVID-19 vaccine it would overlap completely. These are the countries which would be most vulnerable.
How can digital solutions help with diagnosis and treatment?
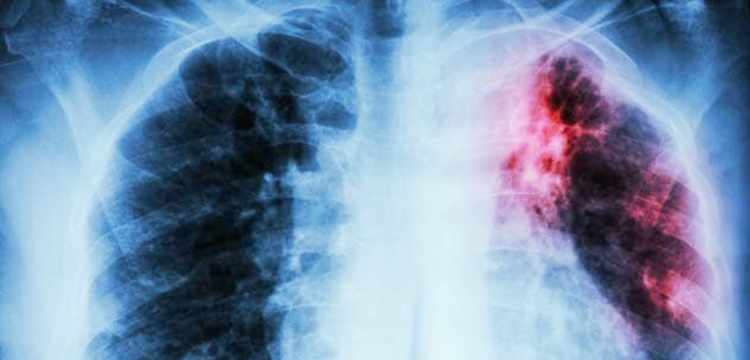
The Stop TB Partnership has been trying to push the use of new innovations and non-traditional solutions for diagnosing TB in particular. Digital technologies and Artificial Intelligence (AI) are extremely useful, especially in X-rays and molecular diagnosis. Digital technology enables doctors who are located in a completely different place from their patient to assess test results and form a diagnosis. AI is also particularly valuable in terms of analysing multiple images, for example of an X-ray or CT scan, in order to form or predict a diagnosis. There are all these innovative approaches: it is the smart way forward in healthcare to implement technology and AI into diagnosis and treatment pathways.
Has the COVID-19 pandemic had an impact on international efforts to prevent and treat TB?
Unfortunately, it has; and this is still happening. There are three key reasons for this: firstly, COVID-19 is an airborne disease, like TB, and it primarily affects the lungs. This has meant that a lot of the doctors and nurses working in pulmonology departments, who had previously been primarily dealing with TB, had to shift their focus from TB to COVID-19. That has had a huge impact, particularly in countries where TB was already a problem. The second reason is that a lot of the hospital departments and beds which had previously been set aside for TB patients were also refocused towards COVID-19. The same has applied to equipment such as the GeneXpert machine, which performs rapid molecular testing for TB, but which has been repurposed in a number of facilities to test for COVID-19. The other key impact has been on funding for TB research and treatment: a lot of attention and financing has obviously been redirected towards COVID-19.

Aside from these factors, lockdown measures have increased the number of barriers facing people with TB: if people are already vulnerable, it has become more difficult for them to get anywhere. People who may have TB are too scared of the risk of COVID-19 to go to the hospital to be diagnosed; this fear of accessing care means that instead of getting treatment, they will stay at home and risk infecting others.
What can be done to address the continued threat of TB at the policy level?
The heads of state and ministers of health in countries with a high burden of TB need to be aware that TB is a big threat not only to their people, but also to their economy. The impact that it has on the economies of countries is really huge. The decision-makers in these countries all signed commitments at the UN High-Level Meeting to end TB by 2030 and to deliver on the key objectives for the end of 2022; and there needs to be a degree of smart thinking to examine what can be done to continue the fight against TB, rather than just focusing on COVID-19.
Civil society and communities at the grassroots are essential for any disease, but they are particularly important for TB. Having groups of community health workers, who are properly equipped, paid, informed and trained, deployed in communities to speak with people; to communicate with them what must be done; encouraging them to seek diagnosis and treatment; and even accompanying them to clinics and supervising their treatment, can be very beneficial.
There are solutions available: India is doing fantastic work in trying to end TB by 2025; there are efforts in a few countries such as Indonesia, Nigeria, the Philippines and South Africa maintaining that TB work. All these efforts start with the people – not only the decision-makers, but also the general population – being aware that in many countries of the world, even taking COVID-19 into account, tuberculosis is still one of the main killers. And that is a huge failure.
